Parkinson’s Disease (PD) is a progressive neurological condition that affects movement, coordination, balance, and muscle control. As symptoms progress, individuals may experience tremors, stiffness, slow movements, and difficulty maintaining balance. While Parkinson’s cannot be reversed, physiotherapy plays one of the most powerful roles in slowing progression, enhancing mobility, improving balance, and helping patients stay independent for longer.
At My Pain Clinic Global, Bandra, Mumbai India, specialised Parkinson’s physiotherapy and neuro rehab programs help individuals regain control over their movements, reduce rigidity, and improve quality of life.
Understanding Parkinson’s Disease and Movement Challenges
Parkinson’s Disease affects the basal ganglia, the part of the brain responsible for smooth, coordinated movements. This leads to symptoms such as:
- Tremors in hands, arms, or legs
- Muscle stiffness
- Slowed movements (bradykinesia)
- Stooped posture
- Shuffling gait
- Poor balance
- Difficulty initiating steps
- Freezing episodes
These symptoms impact everyday tasks like walking, getting out of bed, climbing stairs, and maintaining balance. This is where neuro-focused physiotherapy becomes crucial.
Role of Physiotherapy in Parkinson’s Disease
Physiotherapy helps Parkinson’s patients by improving:
- Balance and stability
- Gait pattern and walking speed
- Posture correction
- Joint mobility
- Muscle strength
- Coordination
- Flexibility
- Movement initiation and control
- Confidence while walking
A structured program helps manage tremors, reduce stiffness, and enhance overall functional independence.
Key Physiotherapy Approaches for Parkinson’s
1. Balance Training
Balance problems are common due to postural instability. Therapists use:
- Static balance exercises
- Dynamic balance drills
- Weight-shift training
- Single-leg support
- Core activation
Improving balance reduces fall risk and enhances confidence during daily activities.
2. Gait Training for Movement Improvement
Parkinson’s patients often develop a shuffling gait. Physiotherapists use:
- Step initiation techniques
- Big-step training
- Visual and auditory cues
- Treadmill gait therapy
- Arm swing coordination
These techniques help regulate rhythm and increase stride length, improving overall walking ability.
3. Tremor Control Techniques
While tremors may not disappear completely, physiotherapy can reduce their impact through:
- Relaxation exercises
- Deep breathing
- Reciprocal limb movements
- Weighted functional tasks
- Strengthening weak muscles
- Proprioceptive feedback
These methods help patients gain better command over daily tasks like writing, holding objects, and eating.
4. Posture Correction and Mobility Drills
Parkinson’s patients often develop stooped posture. Physiotherapists focus on:
- Thoracic extension exercises
- Shoulder mobility drills
- Back strengthening
- Hip flexor stretching
- Spine mobility patterns
Good posture improves breathing, balance, and gait mechanics.
5. Neuro Rehab Exercises
Neuro rehabilitation enhances communication between the brain and muscles. This includes:
- Movement sequencing
- Neuro-motor control exercises
- Bilateral coordination
- Multi-task training
- Cognitive-motor integration
These advanced techniques help patients regain fluid, controlled movements.
6. LSVT BIG – High-Amplitude Movement Therapy
This evidence-based therapy focuses on making movements:
- Bigger
- Faster
- More deliberate
It improves mobility, walking, and daily functional tasks.
7. Strengthening and Flexibility Programs
Weak and tight muscles worsen Parkinson’s symptoms. Strengthening programs target:
- Core
- Legs
- Back
- Arms
Flexibility routines reduce stiffness and allow smoother movements.
8. Functional Mobility and ADL Training
Therapists teach patients how to:
- Get out of bed
- Sit-to-stand transitions
- Climb stairs
- Turn safely
- Maintain balance during daily routines
This improves independence and reduces caregiver dependency.
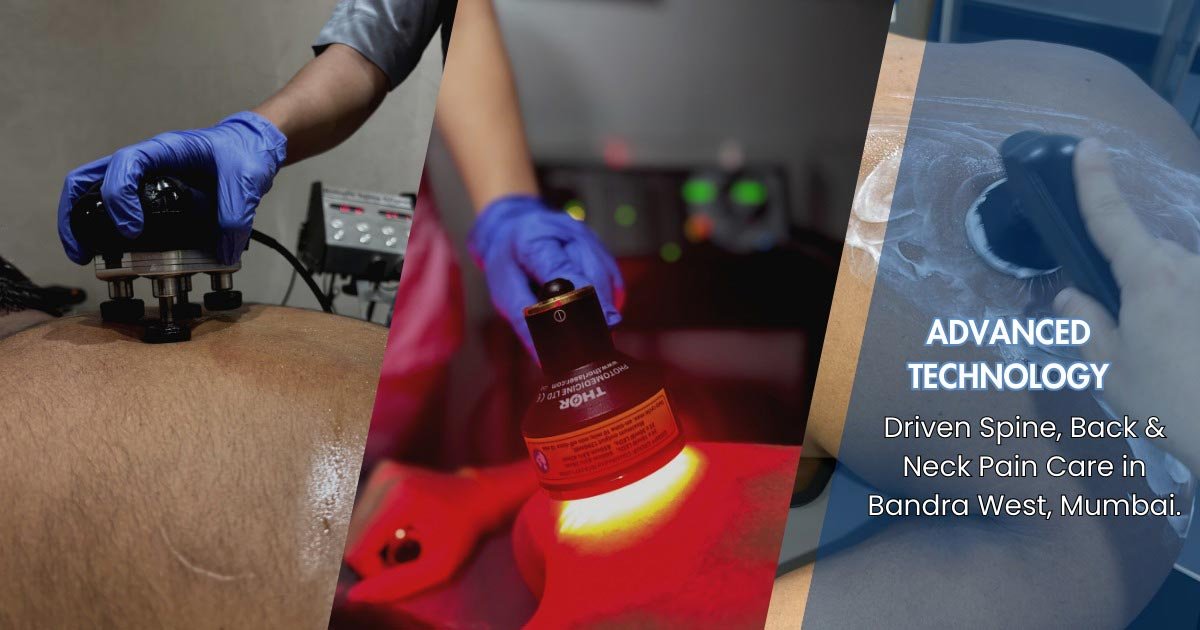
Therapies and Technologies at My Pain Clinic Global, Bandra, Mumbai India
At My Pain Clinic Global, specialised Parkinson’s physiotherapy and neuro rehab programs include:
- Balance correction systems
- Gait and posture analysis
- Robotic-assisted movement training
- Tremor control drills
- Strength and flexibility protocols
- Neuro-motor retraining
- Individualised movement improvement plans
Patients receive one-on-one therapy tailored to their stage of Parkinson’s Disease.
Benefits of Physiotherapy for Parkinson’s Disease
- Improved balance and reduced falls
- Better mobility and walking stability
- Enhanced posture
- Reduced stiffness
- Improved gait and stride length
- Better control over tremors
- Increased independence in daily activities
- Slowed disease progression
- Better confidence in movement
Physiotherapy empowers individuals with Parkinson’s to stay active, mobile, and independent for longer.
When Should a Parkinson’s Patient Start Physiotherapy?
The earlier, the better.
Physiotherapy should begin:
- At diagnosis
- When symptoms first interfere with daily tasks
- After any noticeable decline in walking or balance
- Following changes in medication
Early intervention leads to better long-term outcomes.
Conclusion
Physiotherapy plays a vital role in managing Parkinson’s Disease by focusing on balance improvement, tremor control, movement enhancement, and neuro rehab. With consistent therapy, patients experience better mobility, reduced stiffness, and greater confidence in daily life.
For specialised Parkinson’s physiotherapy in Bandra, Mumbai India, My Pain Clinic Global offers advanced neuro rehabilitation programs designed to maximise mobility and independence.